Combating Methicillin-resistant Staphylococcus aureus
by Oran Payne
Abstract
Methicillin-resistant Staphylococcus aureus (MRSA) is an antibiotic-resistant bacterium becoming prevalent throughout the world. MRSA can be acquired both in health care settings (Hospital-Acquired MRSA or HA-MRSA) and communities (Community-Acquired MSRA or CA-MRSA). To combat this rising public health threat effectively, measures must be undertaken to limit MRSA exposure. This review article examines research focusing on the characteristics of patients with the largest number of MRSA infections to discover who is most susceptible and why. Additionally, the mechanisms for transmission of both HA-MRSA and CA-MRSA are explored. By understanding how MRSA is spread and who is most likely to be infected, public health officials can enact measures to protect the most susceptible populations and to limit the exposure of other groups.
IntroductionMethicillin-resistant Staphylococcus aureus (MRSA) is a bacterium that poses a serious threat to millions of people throughout the world. According to the Centers for Disease Control (CDC), 2.3 million people in the United States were infected with MRSA in 2007, resulting in 19,000 deaths. 1 First discovered in the 1880s, Staphylococcus aureus (S. aureus) is transmitted through direct, skin-to-skin contact with an infected person or through indirect contact with items, such as towels or razors, that have come into contact with infected skin. The resulting infection is characterized by painful skin and soft tissue conditions such as boils, scalded-skin syndrome, and impetigo.2 If left untreated, S. aureus can lead to pneumonia and bloodstream infections, two potentially fatal conditions. During the 1940s, S. aureus became treatable with antibiotic medications such as penicillin.2 However, due to the misuse and overuse of antibiotics in the late 1940s and 1950s, S. aureus became resistant to penicillin. To treat penicillin-resistant strains of S. aureus, methicillin, a penicillin-like antibiotic, was introduced.2
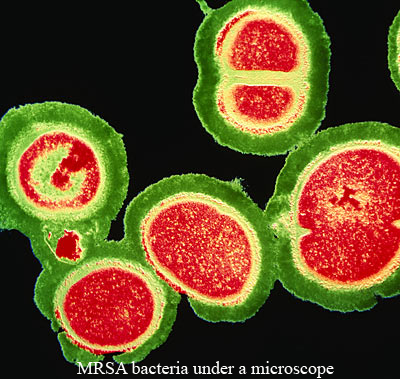
Image Credit: UCLA Newroom, October 17, 2007
In 1968, the first case of MRSA was diagnosed in the United States.2 MRSA infections are characterized as skin infections that lead to red, swollen bumps and are usually accompanied by a fever3; these skin infections can progress to necrotizing fasciitis, a condition that destroys tissue and muscle, popularly known as "flesh-eating disease."4 Over subsequent years, MRSA has evolved to become resistant to the entire class of penicillin-like antibiotics called beta-lactams: penicillin, amoxicillin, oxacillin, methicillin, and others.2 However, a small number of antibiotics can still be used to treat MRSA, although this number is shrinking. Vancomycin, for example, is the antibiotic of last resort for MRSA treatment. Yet, according to the National Institute of Allergy and Infectious Diseases (NIAID), in 2002 the first strain of MRSA resistant to vancomycin was discovered, although this strain is still very rare.2 If this current trend of antibiotic resistance continues, the prospect of MRSA becoming resistant to all antibiotics becomes more realistic, making MRSA an increasingly critical public health issue.
MRSA infections are characterized as skin infections that lead to red, swollen bumps and are usually accompanied by a fever 3; these skin infections can progress to necrotizing fasciitis, a condition that destroys tissue and muscle, popularly known as "flesh-eating disease".
Currently, MRSA can be categorized based on the settings in which patients acquire the infection: hospital-acquired (HA-MRSA) and community-acquired (CA-MRSA).2 The two types of MRSA differ by the common sites of infection/colonization and by their antibiotic resistances. According to the NIAID, HA-MRSA is acquired in health care settings, such as hospitals and nursing homes, due to a number of contributing factors including an increased number of immunocompromised and elderly patients, a rise in the number of invasive procedures (e.g., advanced surgical operations and life support treatments), and failures of health care workers in practicing infection-control measures such as hand washing prior to patient contact and removal of non-essential catheters.2
 |
CA-MRSA is usually acquired within communities by people who have close skin-to-skin contact with others, such as athletes involved in sports such as football and wrestling, soldiers living in close quarters, prison inmates, childcare workers, and residents of long-term care facilities.3 Additionally, people can contract this infection through sharing items that come into contact with infected skin.3 Typically, CA-MRSA only leads to skin or soft tissue infections, but it also can develop into life-threatening infections.
The most effective means of combating MRSA is preventing the infection. To accomplish this goal, the most susceptible populations must be identified to tailor specific measures to protect them. This review article examines studies that analyze cases of both CA-MRSA and HA-MRSA in different hospitals throughout the world to discover the characteristics of patients most susceptible to MRSA. Understanding these characteristics may provide insight into MRSA’s behavior and reveal whether external influences, such as the socio-economic status of patients, play a significant role. In addition, articles that investigate the transmission of MRSA will be examined. The means of transmission is important because it provides information on how to prevent the most susceptible populations from being infected. Since people can be asymptomatic carriers of MRSA, understanding how the infection spreads and who is likely to spread it, in both community and health care settings, will provide valuable information that can be used to institute protocols to reduce the risk of infection.
Identification of CA-MRSA Susceptible PopulationsDiscovering the most susceptible populations can lead to the implementation of specific measures to prevent MRSA infection. Two recent studies at hospitals in Sacramento, California and Houston, Texas aimed to identify the populations with the highest percentage of CA-MRSA infections. In Sacramento, the hospital patients were adults (over the age of 18) and the study covered a seven-month period. In the Houston hospital study, the patients were children (under 18 years old); the study analyzed data over a three-year time span.6 The most prevalent MRSA strain in both studies was USA300, considered by both research teams to be the most common strain of CA-MRSA in the United States.5,6
Discovering the most susceptible populations can lead to the implementation of specific measures to prevent MRSA infection.
After determining the percentage of CA-MRSA cases, both research teams examined various characteristics of infected patients. The Sacramento study focused on gender, age, ethnicity, length of hospital stay, and the type of health insurance. The average age of infected patients was 39 years old; however, the age groups with the highest rate of CA-MRSA infections were aged 18-29 and 40-49.5 Caucasians and males accounted for the majority in each respective category; the average length of hospital stay was only 2.8 days.5 The majority of patients possessed health insurance defined as “public,” which can be assumed to be Medicaid or other government-sponsored programs. In Houston, the researchers focused on the age and ethnicity of the patients. They discovered that children over the age of 10 accounted for the majority of cases; children who were 1 year old accounted for slightly fewer cases.6 African-American children comprised 45.9% of the cases, significantly larger than other ethnic groups.6 According to the 2000 U.S. Census, African-Americans are only 25% of Houston’s population7, which suggests that African-American children are disproportionately affected. Based on the results of these studies, the most susceptible populations seem to be African-American children over 10, and Caucasian males between the ages of 18-29 and 40-49 with public insurance. However, both studies have methodological limitations. Neither study compared the MRSA group to a relevant control group. Also, these studies did not take into account the demographics of the cities in which these hospitals are located.
In addition to the characteristics of the patients, the site of infection and the antibiotics that were effective in each case provide valuable insight into the means of transmission and the emerging trends of resistance. In Sacramento, the most prevalent infection sites were skin and soft tissue, while in Houston the most common type of infection was osteomyelitis, an infection of the bone or bone marrow.5, 6 Since the Houston study covered several years, trends in resistance to certain antimicrobials were evident. The number of cases of MRSA increased each year over the three year period.6 The majority of cases were sensitive to clindamycin, but not erythromycin. However, the number of cases of clindamycin-resistant MRSA increased each year. The same trends can be seen in the data from Sacramento. These studies suggest that clindamycin-resistant MRSA is emerging, but not at an alarming rate.5 Additionally, data on the site of infection reinforce current knowledge about skin-to-skin CA-MRSA transmission. However, in the case of children, more research is needed to determine how to protect children properly from bone or bone marrow infections.6
Identification of HA-MRSA Susceptible PopulationsThe populations most susceptible to HA-MRSA should also be determined to develop specific measures to protect patients. In the Sacramento article, the researchers again focused on the following patient characteristics: gender, age, ethnicity, hospital stay length, and insurance type. They discovered that the average age of HA-MRSA patients was 54, which was 15 years older than the average age of patients with CA-MRSA.5 This finding was reinforced with the age group data that demonstrated that the largest number of HA-MRSA infections occurred in patients over 60, compared to the 18-29 and 40-49 age groups found for CA-MRSA.5 The mean length of the hospital stay for HA-MRSA patients was 21.4 days, nearly 7 times as long as the time for CA-MRSA patients.5 However, similarities between CA-MRSA and HA-MRSA data were found for gender, ethnicity, and insurance type. Males, Caucasians, and those with public insurance comprised the majority of infections for each respective group.5 However, the number of patients with private insurance was almost as high as the number of patients with public insurance. The insurance type is relevant because it could possibly reveal a correlation between MRSA infections and the socio-economic position of the patients. For instance, the Sacramento study indicated that homeless injecting drug users made up 49% of CA-MRSA infections, but only 19% of HA-MRSA cases.5
In the third study, conducted at a Boston hospital in order to discover a link between MRSA and bacteruria, the researchers found that the great majority of HA-MRSA patients were recently hospitalized males, with an average age of 70.7 years.8 These findings were similar to the ones in two other studies that sought to characterize the most common carrier of HA-MRSA. One study, conducted in a hospital in India, focused on discovering the most likely carrier of HA-MRSA in a hospital setting: inpatients, outpatients, or health care workers. The researchers discovered that the main carriers of HA-MRSA were male inpatients.9
In addition to analyzing the characteristics of the patients, all three studies charted the antibiotics that proved effective in treating these strains of HA-MRSA, as well as the sites of infection. The Boston study focused on the presence of HA-MRSA in urine.8 In the Sacramento study, the most common sites of infection were the skin and soft tissue.5 The India study examined the throat, the nose, and the nose and throat together. The nose accounted for the highest number of cases, but there were an equal number of infections in both the throat and nose and the throat alone.9 Both the throat and nose and the throat alone accounted for slightly fewer cases than the nose alone. The site of infection is important because of the severity of the resulting infection. Skin or soft tissue infections are more common, but less invasive than pulmonary infections.5 Additionally, the site of infection provides insight into how MRSA is transmitted and information on where to screen patients and hospital personnel in order to be cost effective. For instance, since the nose is the most common site of infection in the study in India, screening other parts of the body would probably be a waste of money.
Transmission of CA-MRSAEven though the name CA-MRSA implies that the infection is always contracted in the community, there is an increasing frequency of CA-MRSA infections occurring in the hospital. Two articles examined the transmission of CA-MRSA in hospital settings. The first study, conducted in a hospital in Uruguay, examined patients who tested positive for CA-MRSA. The patients were divided into two groups based on the time frame for their CA-MRSA symptoms to appear. If a patient showed symptoms within forty-eight hours of hospital admission, the infection was categorized as community-onset CA-MRSA. If the symptoms were discovered after forty-eight hours, the infection was defined as hospital-onset CA-MRSA. The researchers discovered that not only the number of CA-MRSA infections increased over the two year period of the study, but also that 21% of CA-MRSA cases were hospital-onset.12 Based on these data, the researchers concluded that CA-MRSA is replacing HA-MRSA as the strain commonly transmitted between people in Uruguay and possibly other parts of the world.
Another article analyzed how CA-MRSA spread in the neonatal intensive care unit of a hospital in San Antonio, Texas. The researchers examined cases of CA-MRSA infections among infants and discovered that only 4 out of 676 (0.6%) were infected.11 However, three health workers who directly cared for infants became infected, also resulting in the transmission of CA-MRSA to their family members. Based on these results, the researchers believe that CA-MRSA can spread from patients to health care workers, and then to their families and surrounding communities. To combat this mechanism of transmission, the researchers recommend more vigilant screening of all health care workers, as well as cohorting nurses, patients and supplies. Cohorting is designed so that patients who are infected with a certain strain of MRSA are grouped together and treated solely by a designated team of nurses. Supplies used in treatment are not shared between groups or used in treatment of uninfected patients. The purpose of cohorting is to reduce the risk of hospital workers transmitting MRSA to uninfected patients, other health workers, or infecting MRSA patients with different strains.11
Cohorting is designed so that patients who are infected with a certain strain of MRSA are grouped together and treated solely by a designated team of nurses.
To control the incidence of CA-MRSA, how it is spread outside of health care settings must be determined. A study in Belgrade, Serbia, collected samples from different areas of public transportation vehicles, such as handrails and doorknobs. The researchers discovered that 30.1% of the samples tested positive for the presence of methicillin-resistant coagulase-negative staphylococci (MRCoNS), but all samples were negative for the presence of MRSA.12 Despite the absence of MRSA, however, the presence of MRCoNS is important because it demonstrates the presence of methicillin-resistant bacteria in the community; these bacteria can spread to hospitals. Additionally, the researchers were mostly troubled by the relationship between MRCoNS and MRSA. In the Belgrade study, the MRCoNS were resistant to beta-lactams as well as two other classes of antibiotics due to their evolution in a community setting.12 MRCoNS are able to transfer their genes for resistance to other bacteria, particularly MRSA. Therefore, since MRCoNS can spread to hospitals, there is a significant risk that HA-MRSA, as well as CA-MRSA, can evolve to be increasingly resistant to current antibiotics.1
Transmission of HA-MRSAThe identity of carriers of HA-MRSA remains controversial. Three of the articles collected information on hospital staff, as well as patients, to determine if hospital staff were responsible for transmitting HA-MRSA between patients, or if patients were spreading it among themselves. Additionally, the articles examined the role of health care workers in the spread of HA-MRSA in the community. The San Antonio researchers related anecdotes of two nurses who were HA-MRSA carriers, and subsequently infected their children.11 Thus, health care workers and the families of patients infected with HA-MRSA are able to spread it to the community.
The three articles examined health care workers who tested positive for the presence of MRSA. In the India study, the researchers collected samples from the nasal cavities of 200 subjects, including 57 hospital workers. They discovered that only 1 out of 57 (1.8%) health care workers tested positive for the presence of MRSA, which differs significantly from other studies that indicated that 6-50% of health care workers were carriers.9 In a study conducted in Palestine, the researchers examined the transmission of CA-MRSA in hospital settings. They discovered that fifteen out of seventy-two (20.8%) health care workers were positive for the presence of MRSA.13
A study in a hospital in Brazil focused exclusively on S. aureus infections in health care workers. The researchers categorized the health workers by gender, age, professional activity, sector, shift, length of time in profession and sector, the use and number of individual protection equipment (IPE), and the number of hospitals worked in. They discovered that women, workers between the ages of 20 and 28, day shift workers, workers in ICUs and surgical wards, and workers who have been in the profession for less than seven years and who have been in a sector less than two years all had the highest rates of colonization.14 The researchers in this study discovered that nurse technicians who worked in multiple hospitals and used one IPE sporadically had the highest number of positive tests for the presence of S. aureus.14 Despite the large number of S. aureus infections (52 out of 202), however, only three of them were categorized as MRSA infections.14 Based on these results, the researchers concluded that health care workers are not significant contributors to HA-MRSA infections.
In contrast to the India report, the Palestine researchers reported that the average number of infected health care workers was 4.6%, which is toward the bottom end of the spectrum reported in the India report.13, 9 However, the Brazil report estimated the average percentage of MRSA-infected health care workers in the world to be between 17% and 40%.14 This significant amount of variance is due to the differences in regions, as well as the differences in hospital protocols.
However, in all three studies, the patients had the highest number of infections, and thus were considered the primary source of HA-MRSA transmission. The vast differences in rates of infection among health care workers in these three reports lead to different protocols enacted in hospital settings. If the health care workers are a significant cause of HA-MRSA, then additional infection control measures for staff need to be instituted in hospitals and other health care settings. One solution offered by the researchers in India is to perform nasal screening of both patients and health care workers in hospital areas with the highest rates of infection, such as burn and dermatology units, where the rate of colonization and infection is high.9 If the health care workers are not considered a significant source of infection, then only the patients should be screened.
ConclusionThe articles examined in this critical review provide important information that can be used to effectively combat both types of MRSA. HA-MRSA mostly affects older patients (people over 60), while CA-MRSA affects people who are, on average, younger adults (39 years old). The role of health care workers in the transmission of both types of MRSA remains unclear. The articles reviewed here claim that relatively few health care workers are colonized; however, the articles that they cite offer significantly different numbers.
These data provide starting points for further research to determine why these populations are susceptible. For instance, the overwhelming number of males infected with both types of MRSA led one group of researchers to suggest that MRSA infections may be related to hormones.11 The means of transmission also provides important information. In the case of CA-MRSA, more research is needed to understand why it is emerging as the dominant MRSA subgroup in certain hospitals and if this trend will extend to other regions. Also, further research is needed to affirm the results of researchers who examined public transportation vehicles for the presence of CA-MRSA. One such experiment should be the examination of public transportation vehicles, such as subways or shuttles that exclusively service hospitals. The purpose of this study would be to gauge how far CA-MRSA travels outside the hospital and if hospitals are contaminating the surrounding community.
For HA-MRSA, better protocols that group carriers and the infected together, as well as more stringent policies regarding the interactions with the infected, including the use of IPEs, are needed. All of the articles suggest that following current guidelines regarding MRSA prevention, such as constant hand washing and abstaining from sharing any items that may come into contact with others, will help prevent the spread of CA-MRSA.2 To combat HA-MRSA effectively, hospitals need to implement stricter guidelines, such as grouping patients together by the strain of MRSA, screening hospital personnel, and isolating infected patients from others, as well as ensuring that personnel who work with infected patients do not work with the uninfected.9,11 By understanding what causes people to be at risk for infection, as well as how the infections are spread, MRSA may be able to be controlled.
Works Cited
- S. aureus and MRSA Surveillance Summary 2007." 17 Oct 2007. Center for Disease Control and Prevention. 24 Apr 2009 http://www.cdc.gov/ncidod/dhqp/ar_mrsa_surveillanceFS.html
- "Methicillin-Resistant Staphylococcus aureus (MRSA)." National Institute of Infectious Diseases. . Web.24 Apr 2009. http://www3.niaid.nih.gov/topics/antimicrobialResistance/Examples/mrsa/history.htm
- National MRSA Education Initiative: Preventing MRSA Skin Infections." Centers for Disease Control and Prevention. . Web.24 Apr 2009. http://www.cdc.gov/mrsa/mrsa_initiative/skin_infection/mrsa_faqs.html
- Smith, Michael. "IDSA: MRSA Linked To Necrotizing Fasciitis." MedPage Today. 12 Oct 2006. 14 May 2009 www.medpagetoday.com/MeetingCoverage/IDSA/4278
- Huang Hsin, Flynn NM, King JH, et al. Comparisons of Community-Associated Methicillin-Resistant Staphylococcus aureus (MRSA) and Hospital-Associated MSRA Infections in Sacramento, California. Journal of Clinical Microbiology. 2006:2423-2427
- Kaplan SL, Hulten KG, Gonzalez BE, Hammerman WA, et al. Three-Year Surveillance of Community-Acquired Staphylococcus aureus Infections in Children. CID. 2005;40:1785-1791.
- McKinnon, Jesse. "The Black Population: 2000." Aug 2001. U.S. Census. 24 Apr 2009 http://www.census.gov/prod/2001pubs/c2kbr01-5.pdf
- Routh JC, Alt AL, Ashley RA, Kramer SA, and Boyce TG. Increasing Prevalence and Associated Risk Factors for methicillin Resistant Staphylococcus Aureus Bacteriuria. The Journal of Urology. 2009; 181:1694-1698.
- Mathanraj S, Sujatha S, Sivasangeetha K, Parija SC. Screening For Methicillin-Resistant Staphylococcus Aureus Carriers Among Patients and Health Care Workers of a Tertiary Care Hospital in South India. Indian Journal of Medical Microbiology. 2009; 27:62-64.
- Benoit SR, Estivariz C, Mogdasy C, et al. Community Strains of Methicillin-Resistant Staphylococcus aureus as Potential Cause of Healthcare-associated Infections, Uruguay, 2002-2004. Emerging Infectious Diseases. ; 14:1216-1223.
- McAdams RM, Ellis MW, Trevino S, and Rajnik M. Spread of methicillin-resistant Staphylococcus aureus USA300 in a neonatal intensive care unit. Pediatrics International. ;50:810-815.
- Stepanovic S., Cirkovic I., Djukic S., Vukovic D., and Svabic-Vlahovic M. Public transport as a reservoir of methicillin-resistant staphylococci. Letters in Applied Microbiology. ; 47:339-341.
- Kaibni MH, Farraj MA, Adwan K, Essawi TA. Community-acquired methicillin-resistant Staphylococcus aureus in Palestine. Journal of Medical Microbiology. 2009; 58:644-647.
- Ferreira da Silva ECB, Antas MGC, Neto AMB, et al. Prevalence and Risk Factors for Staphylococcus aureus in Health Care Workers at a University Hospital of Recife-PE. The Brazilian Journal of Infectious Diseases. ; 12:504-508.
 Oran R. Payne is the younger of two children and originally comes from South Berkeley, California. He graduated with the MIT class of 2009 and majored in Chemical-Biological Engineering. His inspiration for writing this piece was his previous work with bacteria and articles he read in the newspaper.
Oran R. Payne is the younger of two children and originally comes from South Berkeley, California. He graduated with the MIT class of 2009 and majored in Chemical-Biological Engineering. His inspiration for writing this piece was his previous work with bacteria and articles he read in the newspaper.