
| Vol.
XXII No.
4 March / April / May 2010 |
| contents |
| Printable Version |
MIT Medical Director Discusses Changes:
Community Care Center Proposed
The following discussion between MIT Medical Director William M. Kettyle (WMK) and the Faculty Newsletter (FNL) took place on April 21 of this year.
FNL: You are proposing some changes in services at MIT Medical. Over the past few years there have been some service changes and others are proposed. Are these changes in response to the budgetary pressures experienced at MIT and in our economy?
WMK: We have continued to strive to use our resources here to the fullest. Indeed, at Medical and across the campus fiscal constraints are a reality. We have tried and strived to make sure that these limitations have had and will continue to have the least impact on patient care. We also need to make sure that our care systems evolve with advances in care and meet the needs of our community. Some of the changes reflect evolution of care systems and changes in the practice of medicine in our community, and others are in response to budgetary pressure.
FNL: You have proposed discontinuation of overnight, on-site care. Can you explain the proposal and tell us how this proposal was developed?
(click on image to enlarge)
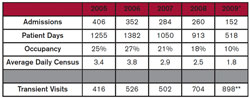
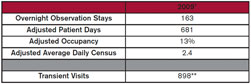
WMK: Over the last several years there have been significant changes in the utilization of our Inpatient Unit. We have seen the number of admissions decline significantly. Over the past five years there's been a persistent reduction in admissions. During this same time period there has been a dramatic increase in what we call "transient visits.” These are visits to the Inpatient Unit that don't involve an overnight stay, but do involve the provision of care – care that is in keeping with changes in the delivery of services and the management of medical conditions. The administration of intravenous fluids and drugs, dressing change, administration of other injectables, teaching, etc. We have seen a significant increase in the utilization of our facilities and personnel for care episodes that are not admissions.
(click on image to enlarge)
This change in usage parallels important developments in the flow and mechanics of care in the medical environment around us. Hospital stays have gotten shorter. There are increasing, high quality resources available in our community to provide care at home or at a living facility. There have also been significant changes in medical care that allow the treatment for certain conditions to be done as an outpatient rather than as an inpatient. For example, there are antibiotics that can be given once a day instead of three or four times a day. We now have drugs to treat blood clots that can be given by the patient to himself or herself rather than via an intravenous drip. The availability of home physical therapy and occupational therapy is also reflected in a significant decline in the utilization of the Inpatient Unit for post illness or post-operative rehabilitation.
In addition, many of our senior members are moving to living facilities where extended care or assisted living services are available. Home hospice services have improved significantly and for many patients home is the most comfortable place for care at the end of life and we have seen a significant decrease in the utilization of our unit.
We've been aware of these changes in usage and have been and still are looking for ways to utilize our personnel and our bed space to maintain an appropriate use of our resources, to cover the fixed costs of having the Inpatient Unit remain open.
Options explored to defray the fixed costs of providing care in the Inpatient Unit have included the following:
• Shorten acute hospital stays by transferring patients to the Inpatient Unit – thereby decreasing acute care hospital costs. (The mechanics include “payback” methodologies based on hospital payment arrangements.)
• Commercial research – drug trials
• Respite/post-op care (aka “The Charles Hotel model”).
• Sleep studies
• Hospice care (in coordination with the MGH)
• Colonoscopy center
• Rehabilitation facility
After feasibility review, none of the above has been practical enough to operationalize. In addition we have, for the past several years, been staffed at what we feel is the minimal level to support high quality care – decreasing staffing without changing services is not an option.
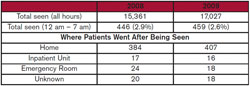
(click on image to enlarge)
Our proposal also includes some changes in our Urgent Care service. The Urgent Care area provides walk-in and same-day appointment service for all those eligible to use the MIT Medical Department. The visit volume varies widely, with the late afternoon and evening being the busiest times. After 11:00 pm the frequency of visits decreases significantly. The vast majority of the visits seen during the night (midnight – 7:30 am) are of the convenience kind (“I’m still up and I've had this X [where X = cold or rash or sore knee] for several Ys [where Y = days or weeks or months]”). During the night and in some cases during regular business hours, visits of a truly emergency nature are triaged by phone or, after a brief initial assessment, sent to an acute care hospital emergency room with a larger range of diagnostic and therapeutic services – X-ray, CT scanning, emergency room level care – for fractures, other trauma, heart attacks, abdominal pain, high fever, etc.
The proposal we are putting forth is to rebalance the deployment of our resources. We want to increase and augment services of the “transient visit” kind and support this enhancement with resources that are currently underutilized.
| Back to top |
The Proposal
Create a Community Care Center – staffed by nurses trained in care management who will be knowledgeable regarding the availability of resources, who can coordinate and monitor the delivery of services. This team of nurses will also provide the nursing care services for the “transient visits." The potential for involvement of these nurses with living units and segments of our community will enhance care and likely improve outcomes. The Center would be open from 7:00 am until 7:00 pm on weekdays.
• Discontinue overnight services in the Inpatient Unit. One of the important responsibilities of the Community Care nursing team will be to help arrange alternative care plan for those who historically would have spent the night in the inpatient unit.
•Continue to provide Urgent Care Service from 7:00 am until 11:00 pm. This would provide convenient, on-site care for mild-to-low acuity problems. Overnight we will arrange access to local emergency room facilities.
• Engage a triage call system, staffed by trained nurses following accepted protocols to provide advice when our facility is not staffed. From 11:00 pm until 7:00 am this dedicated service, a service that is aware of the available resources, will provide advice and instructions.
The proposal is indeed a work in progress. Our plan is to build the Community Care Center and provide the enhanced services before making any changes in the availability of on-site, overnight services.
Our current overlap horizon extends until the end of the calendar year. We are making a major effort to engage community input and have talked with faculty, departments, and student groups – seeking comments, suggestions, input.
FNL: The Inpatient Unit was closed for two months over the summer. Why was this done and what was the impact on care for our community?
WMK: Inpatient utilization is very low during what we call the summer – roughly June 15 until August 15. In addition to decreasing our personnel expense, this closure gave an opportunity to evaluate our Community Care proposal. The summer of 2009 experience demonstrated that closing the Inpatient Unit overnight and closing the Urgent Care area from midnight until 7:30 am resulted in no measurable increase in emergency room visits or hospital admissions (based on insurance billing data) and we are not aware of any adverse effect on the quality of patient care or problems related to the overnight closings. Prior arrangements were made with Mount Auburn Hospital to offer care and to facilitate the continuity of care for members of our community needing services during the night. In addition, the telephone triage service I described earlier was put in place with excellent acceptance by both patients and clinicians.
FNL: Will the proposed changes result in significant cost savings?
WMK: Our proposal, in fact, involves spending more in some areas and less in others. The net annual saving – after spending more in some areas and less in others – is about $1 million or ~ 2.5% of our annual operating budget. The cost savings are significant, but the opportunities to enhance the care we provide and more efficiently use our resources are the major components of the proposed changes. Having highly trained nurses and doctors remain idle during the night is not ideal professionally or fiscally.
FNL: How will members of our community obtain care during the night?
WMK: That depends upon what they need. For many patients the daytime activities in the proposed Community Care Center will have included arrangements for overnight care, if needed. That could include supportive services at home or transfer to another medical facility. Building on long and strong relationships with area health care facilities we are exploring arrangements that will facilitate the transfer of patients requiring inpatient level of care.
The urgent challenge is really in the realm of providing students with care overnight. Gastroenteritis, mononucleosis, alcohol intoxication, often require prolonged intravenous fluid administration and or supportive care. We are currently in negotiation with Mount Auburn Hospital and with their hospitalist services to provide bed space for students for overnight care in situations like those mentioned. We are also exploring an arrangement with Harvard University Health Services. For MIT Health Plan members and retirees, our long-standing relationships with both Mount Auburn Hospital and the Massachusetts General Hospital will not change significantly. We will, however, be more involved and active in discharge planning for patients hospitalized at these or any of the other local facilities.
FNL: How will a Heath Plan member, student, or retiree know what to do or where to go in an emergency situation?
WMK: Call. Calling our number to access care will automatically connect them with our staff or our triage service. Overnight advice might also include contacting the MIT clinical on call. Internal Medicine, Pediatric, OB/Gyn and Mental Health clinical will remain on call 24/7 under the proposed system and will be available to patients via the call system. Mental Health services will continue to be available 24/7. The venue for overnight mental health, face-to-face evaluations is being determined.
The nocturnal call service will report all calls and advice given at 7:00 am the next day. A member of our Community Care Center team will review the log of calls and provide follow-up care, advice, facilities appointments, etc.
The Call Center nurses are trained to provide advice to those seeking help for a medical condition, injury, or other concern. For some callers the advice might be:
“It sounds like this could wait until later in the morning. I will let the Community Care Center team know that you called. How can they best reach you at about 8:00 am?”
Or
“Try to get the fever down with some ibuprofen – take two (200 mg., each) now and again in about four hours, drink plenty of fluids. I will let the Community Care Center team know that you called. How can they best reach you at about 8:00 am?”
Or
“I think you need evaluation tonight. Please go to the Mount Auburn Emergency room…..they are located at……I will call them and let them know you are on your way…I will also let the Community Care Center team know about this call and they will follow up with the hospital and with you. . . .I hope you feel better soon. . . .”
FNL: How will those needing care get to the emergency room?
WMK: That depends on the illness, the acuity, and the locally available resources. An ambulance is the way to travel for any one with a severe, unstable, or uncertain condition. Our on-campus student-run EMT service is excellent. When the MIT EMT service is not on duty, or for off-campus needs, professional ambulance services should be engaged. The triage service will know what resources are available. For less acute transportation needs a taxi or private car are probably the most realistic forms of transportation. For students we will provide cab services.
FNL: What are the cost issues for someone referred to an emergency room overnight?
WMK: An emergency room visit suggested by the overnight phone service would likely have been an emergency room visit in any event – even if we had overnight services here at MIT. High acuity, urgent care situations do now require and will continue to require hospital-level emergency room care. The co-pay system for this type of care would remain unchanged.
For a student, co-payments would be borne by the Medical Department or by the student’s insurance, depending on the diagnosis, the acuity, and the care needed.
For most members of our community there will not be a significant change in out-of-pocket costs.
| Back to top |
FNL: Are there other changes in clinical services that are slated for the MIT Medical Department?
WMK: There are two other changes that have been put in place.
We have had 18 different dermatologists here in the last five years. This presents a significant issue administratively and clinically. Because of this and because we have seen a significant increase in the availability of high quality, nearby, off-campus, dermatologic services, we have decided not to have a dermatologist on site. We will continue to have an on-site dermatologic nurse specialist.
One other change is driven by changes in technology. We will no longer be doing echocardiograms on site. Our equipment needs to be updated and the number of studies we do does not support the purchase of the latest equipment. We have easy access, with relatively short queues, to state-of-the-art echocardiography at three or more different facilities in the area. There will be no change in the billing for echocardiography.
FNL: At our last interview we discussed broadening the use of the MIT Medical facilities for member of the community who are not students or MIT Health Plan members. Has this materialized?
WMK: We are continuing to put into place operational changes that will support this valuable endeavor. There has been a slight increase in the utilization of our facilities by members of our community who are not students or Health Plan members. We are continuing to work toward increasing this utilization.
FNL: Can you provide us with an up-date on your community mental health outreach activities?
WMK: We are continuing a number of activities to increase awareness of service, decrease stigmatization, and help identify those who might benefit. There have been no reductions in our mental heath services. The proposed changes in overnight services will not affect our mental health care activities. We continue to be actively involved in reaching out to our campus community with regard to mental health needs. We are also actively screening members of our community for depression and other significant mental health issues.
FNL: The focus of the Mental Health Service appears to be on student care. How is that going?
WMK: We have indeed increased our focus on students at our mental health service. We are seeing more students and I think our outreach efforts are effective. This is a very important component of our medical service and we will continue to support these endeavors.
FNL: Co-pays have been initiated for some services. How was that decision made and why are these necessary?
WMK: We have long avoided co-pays. The reasons to avoid them are many and most are obvious. Changes in legislation have forced us to add co-pays for certain services. The concept of mental health parity is based on the premise that mental health conditions should not be managed differently than medical conditions. We have had co-pays for psychiatric or mental health services, and in order to comply with mental health parity laws, we have added co-pays for other specialties. We decided to consider mental health services as a specialty and along with other specialty services have put a co-pay system in place. There is no co-pay for services that we consider “primary care.” Internal medicine, pediatrics, obstetrics and gynecology are considered primary care services and co-pays do not occur in those areas. Specialty consultations do involve a co-payment. The co-payment is $10 across the board for specialty services – this means a decrease in mental health co-payments, but an increase in subspecialty co-payments otherwise.
There are no co-pays for most student services obtained at the Medical Department.
FNL: Will there be changes in the Dental Service?
WMK: Our dental service has continued to evolve in several ways that provide outstanding support for the MIT Community. We are now “dentally digital.” Our x-rays, record keeping and billing are all done electronically. Productivity has increased and we have aligned our mix of on-site services to maximize convenience for our patients. For most dental needs, our department can provide all the services.
FNL: During the current fiscal year several members of your staff took unpaid furloughs. Is this part of your fiscal management plan going forward?
WMK: Several members of our department are taking or have taken furloughs to decrease our personnel expenses for the current fiscal year. The furloughs were scheduled to minimize impact on patient care and vital operations. When we decided that furloughs would be part of our reaction to the fiscal pressure we faced, we realized that this was a temporary, short-term, and hopefully not shortsighted approach. We used this mechanism to buy time, to make plans that would enable us to preserve care systems and to minimize personnel reductions. We do not plan on any furloughs for the coming fiscal year and beyond.
FNL: How much has your budget been cut over the past two fiscal years?
WMK: During Fiscal Year 2010 we experienced approximately a 5% reduction in resource availability. For Fiscal Year 2011 we are proposing a further reduction of approximately 2.5%.
FNL: Has your staffing changed significantly?
WMK: Nearly 300 people work at MIT Medical – some are employees and there are a number of contractors. There have been and will be some small reductions in force, but in most areas our workforce is incredibly stable – except in dermatology – we have had a very low turnover rate.
FNL: How much influence did you have on your budget for Fiscal Years 2010 and 2011? Were you given a firm, fixed reduction target?
WMK: We worked closely with the senior administration and Finance to look carefully at our resource utilization. Over the past several years we have put in place robust fiscal monitoring and management systems, and because of this today we have a much better handle on our resource utilization.
We paid careful attention to the work of the MIT Task Force and actively worked internally to find ways to make sure our resources were being effectively used. The work of the Institute-wide Task Force decreased the reduction burden for our department and other departments at MIT. We also actively worked internally to find ways to make sure our resources were being effectively used. These activities rendered some savings. We shared our work, our numbers, our assessments, and our plans with the senior administration and came to an agreement on how much we could reasonably plan to spend for Fiscal Year 2011. So in essence it wasn't a negotiation; it was collaboration – a collaboration focused on maximizing the use of our resources, and maintaining, as much as possible, the convenient, on-site, high quality service that we have traditionally offered.
FNL: Will the new federal health care legislation have a significant impact on MIT Medical and the health plans that it sponsors?
WMK: We are carefully looking at the potential effects of national health legislation on our insurance programs and care systems. One important change is the expansion of coverage up to age 26. This may lead to a decrease in enrollment in our student extended plan. Since we have not had significant benefit limits or eligibility issues in our plans, some of the other components of the health care reform act will not have very much effect on us. Clearly the final form is unclear and the impact on the Institute and our community is being evaluated.
FNL: Are you optimistic about MIT Medical in the future remaining the valuable Institute resource it is?
WMK: Looking forward – we are indeed quite optimistic about our ability to provide high quality, convenient, on-site care. The changes we propose -- the formation of a Community Care Center and the reduction of on-site services overnight – will allow us to continue to provide high quality, convenient care for our community. Working with MIT leadership and with the communities at MIT we will find ways to meet the clinical needs with the resources available.
Thank you for the opportunity to share this information with you and with your readers.
| Back to top | |
| Send your comments |
| home this issue archives editorial board contact us faculty website |