Project Amazonia: Solutions - Indigineous Health Care (OPNAH)
Project OPNAH: Organization for the Protection of Native Amazonian Health
I. Problems:
- Serious diseases and illnesses afflict indigenous groups of the Amazon.
- Many Amazonian Indigenous groups lack affordable health care.
- Some indigenous people lack adequate modern health care education.
- Indigenous people often lack access to basic health care supplies.
- The actual health status of indigenous groups in many areas of the Amazon is undefined.
- Known indigenous groups are currently at varying levels in terms of healthcare needs.
- Current aid programs are helpful, but for the most part, not widespread, and rather disjointed.
II. Plan:
Project Amazonia recommends setting up an experimental independent organization, backed by funds from both the government and other aid organizations, responsible for combating the problem through the following tasks:
- Setting up accessible humanitarian healthcare and health education
- Sending task forces into indigenous territories to investigate need on a case-by-case basis.
- Collaborating with the many current aid projects/ organizations currently situated in the region, in an attempt to create a more cohesive method of aid.
III. Background:
The indigenous people of Brazilian Amazon Rainforest are an integral part of the region, having lived there for thousands of years. In addition to being an intrinsic characteristic of the forest itself, they also represent the greatest source of knowledge of the region. For example, many believe that indigenous people may have incredible knowledge about Amazonian vegetation, including possible medicinal properties that might, in fact, be so strong, that they contain the key to curing such diseases as cancer. Unfortunately, however, many Amazonian indigenous groups are at risk of extinction if the necessary attention is not provided. The people are afflicted with a variety of severe diseases including typhoid, dysentery, influenza, malaria, dengue, minimata, tuberculosis, yellow fever, and measles. Without proper treatment, many of these diseases have fatal consequences, and, much of the time, adequate treatment does not reach these groups. Brazil’s indigenous will eventually perish if the proper actions to protect them from disease are not administered.
There are multiple causes for the indigenous health
crisis. The diseases were first introduced to the indigenous people through
the influx of foreigners from Europe and Africa in the 1500s when Brazil
was “discovered.” As intrusion into the forest has continued, logging
practices have also contributed to the propagation of disease. Minimata
disease, for example, affects the nervous system causing uncontrollable
shaking, muscle wasting and birth defects. The disease is produced by
methyl mercury poisoning, a toxic substance used to separate gold and
ore. In a recently performed study, thirty percent of small-scale Brazilian
gold miners, referred to as “garimperos” had mercury levels in their body
above the World Organization’s standards1. Mining processes
have produced other health risks as well. In addition to methyl mercury,
cyanide released by large-scale mining companies also serves as health
risks to indigenous groups. The seriousness of the issue can be demonstrated
by the1980s discovery of gold in the northern Brazilian state of Roraima.
According to Survival International, a London–based indigenous support
group, within seven years of contact, 20% of the Yanomani population of
the Roraima died from contact-related illness and disease.2
More indirect health problems have also resulted from
contact with outsiders: particularly missionaries, rubber extractors,
gold miners and logging companies. When these foreigners exchanged goods
for cheap labor, the indigenous habituated to the commodities they supplied.
As this reliance developed, it proved harmful to cultural practices, and,
in turn, to the health status of afflicted tribes. The Katukina tribe,
who inhabit the flood land area of the upper Amazonian region, for example,
succumbed to high levels of malnutrition, anemia and vitamin deficiencies
as males began to work away from the villages to attain these industrialized
supplies.3 As a result, malaria, measles, and influenza outbreaks
have afflicted the Katukina tribe.
The indigenous people are especially vulnerable to disease
because of their aboriginal tendencies. According to the Pan American
Health Organization, the tuberculosis rate was ten times Brazil’s national
average. In 1996, malaria was determined to be the main cause of death,
and infant mortality rates were three times the national average. The
situation is not irreversible. Within one year of intensive prevention
and treatment programs, child mortality dropped by sixty percent and deaths
from diseases (malaria and TB) diminished by half.2 However,
as displayed in the following map, based on data collected in 2002, the
risk of malarial infection is still high, and there is still work to be
done:
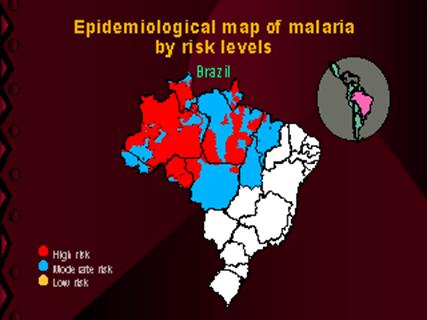
(Courtesy of the Pan American Health Organization)
Health care thus continues to be extremely valuable
in saving many from suffering.
Basic health care in most regions of the Amazon is performed
within the tribes themselves. Societies typically rely on the traditional
medical practices of each individual tribe as their prime source of care.
This is partly due to the fact that many of these communities, such as
that in the Ilhas de Abaetetuba region of the Amazon estuary, suffer from
the effects of a “boombust economy.” In this situation, a large influx
of immigration is followed by a slow or even stalled economy, in which
health resources frequently become scarce and expensive.4 The
second, and perhaps more distinctive problem, seems to be the fact that
effective healthcare is often too distant. In Reeve’s study, out of 80
individuals interviewed from the Illhas de Abaetetua region, the most
common response to the question of seeking medical exams in clinics was
that this method of healthcare was only used as a last resort.2
Another common sentiment among those interviewed was the fact that traditional
treatment worked better because of the faith that the natives are able
to have in its powers. Thus, in creating any health care plan to aid in
indigenous life, it is incredibly important to integrate traditional beliefs
and practices with any western treatment.
The current key players in providing additional healthcare
to the region are the government funded, non-profit organizations, the
Brazilian government itself, and other non-affiliated humanitarian groups.
One notable government-funded group is URIHI, a non-profit group set up
to provide health services to remote Yanomani communities (the term means
“forest” in the Yanomani language). According to a report in OneWorld
US, by Alison Raphael, the group was successful after it’s first year,
with child mortality dropping by 60% and adult death from local diseases
dropping by half.2 This smaller scale effort geared towards
the Yanomani people seems to indicate that a large scale, widespread,
and sustained effort at disease eradication would indeed prove successful.
The Brazilian government also has its own indigenous
health policy. While formerly controlled by the National Health Foundation
(Funasa), as of early 2002, the policy came under the direction of The
Indigenous Health system and the Federal Agency for Disease Prevention
and Control (APEC).5 In the past, the Brazilian government
has stepped up efforts to control the spread of serious diseases in the
Amazon region. According to a report by the World Health Organization,
as of 2001, Brazil increased funding for national disease control in the
Amazon to $54 million US dollars. That year, the number of cases of malaria
in the Brazilian Amazon dropped 43%, from 420,000 in the first eight months
to 237,0000.6 Again, this example seems to support the correlation
between humanitarian aid and widespread health improvement. However, Brazilian
government funding for indigenous groups still seems to be disproportionate
to that of the rest of the population. According to a report by the United
Nations Association for Great Britain and Northern Ireland (UNA-UK), the
annual amount spent by the Brazilian government on indigenous health care
is about R$22 per capita, versus the R$100 per capita Brazilian average.2
A major humanitarian organization that works with various indigenous concerns,
including health care, is Operação Amazônia Nativa
(OPAN). This organization was founded in 1969 and works in the northern
and central-western areas of Brazil.2 The organization sends
groups of four specialized individuals, one of which oversees health concerns,
into a region or society to work on small projects. They are currently
working on five projects in the Amazon, and former material and health
aid seems to have provided success for individual tribes involved. However,
while the organization does seem to be a valuable asset to health care
concerns, its major focus seems to be more on general indigenous rights
than on specific health problems. Thus, the project seems to be a good
starting point for health issues, but does not represent a comprehensive
health plan for the Amazonian indigenous groups.
The major problems associated with these formerly instituted plans seem
to be first, in a lack of sustained dedication to the effort and second,
in a scope that is too narrow for substantial health recovery. The Mission
2006 Plan aims to amend these problems, while still maintaining the successful
aspects of the current health plans.
IV. Procedure: Project OPNAH
a) Presentation of OPNAH to the public (about 5 mo.): OPNAH representatives will present plans to representatives from various affiliated groups, including:
- Brazilian government
- Brazilian organizations: including OPAM and URIHI
- Other organizations: including the World Bank, the UN, the Pan-American Health Organization, and other health oriented groups (This includes visiting small aid groups already in the region for additional input.)
- Indigenous groups of the Amazon: This involves entry into the region to speak with indigenous people about resources that will be offered through the plan. *Note: all services offered will be completely optional and will be provided on a case by case basis depending upon both need and desire for aid* Groups will be asked for input on other possible needs. Indigenous groups can include, but are not limited to the Guarni, Caingang, Ticuna, Terena, Guajajara, Xavante, Yanomami, Macuxi, Potiguara, Xacriaba, Fulni-o, Canipuna, Pata xo, Macuxi, Kuikuru, Baniwa, Mekranoti Kapo, Txu Kahamae, Arapaco, Wari, and Uru-Eu-Wau-Wau tribes.
b) Initial Analysis for permanent clinic sites (about 5 mo): OPNAH representatives enter the Amazonian region and do extensive research and investigation into location sites of each of six clinics scattered throughout the Amazonian state of Amazonas, which has been chosen because of its large indigenous population and central location. Factors in choosing site locations for the clinics will include:
1. Accessibility:
(a) These clinics will also act as supply centers to the region. Thus, accessibility to more modernized areas without disruption of the external environment is a must.
(b) An optimal region will provide easy access to as many needy indigenous groups as possible. *Note: This is a need-based plan. For those rare groups that have ready access to medical care, the service should not be necessary at such a strong level. *
2. Disruption: OPNAH representatives must analyze each region for possibilities of environmental disruption associated with construction.
3. Overall viability: OPNAH representative will analyze the practicality of putting a base station in each considered location. Also, the OPNAH will be responsible for determining a location that is near indigenous groups that actually want aid.
c) ALSO IN YEAR ONE: Recruitment and Remote Aid:
1. Representatives that are sent to interview indigenous groups as part of the Presentation aspect of the plan will also be doctors. They will come with enough supplies for approximately one year, and will supply remote aid to each group that they visit.
2. Recruitment: Approximately four doctors will be required for each of the main clinics, with as many additional volunteer medical workers and doctors as possible. Optimally, most doctors will be Brazilian, and have a firm background in any indigenous languages necessary. One doctor and one health volunteer will also be hired for six mobile clinics working out of each stationary clinic (outlined in more detail later). Volunteers can work over intervals of 2 months, 6 months, or 1 year. Some volunteers can work through programs similar to that in the United States, which gives free medical school tuition in return of service.
d) Construction: (approximately one year)
1. Two OPNAH clinics will be constructed in what is determined to be the most urgent of the six predetermined possible locations. Funding will potentially come from government funds already designated for indigenous health, and/or from funds from other organizations that have been contacted during Presentation.
e) Implementation: (approximately three years): OPNAH will provide services to afflicted tribes, working out of the predetermined clinics. A board of directors comprised of medical representatives from each clinic, who will collaborate at least once a month, to determine necessary changes to the project, and discuss other problems that arise, will oversee the program. OPNAH will provide the following optional services:
1. Basic health care provided at the clinic
2. “Ambulance service” provided by the clinic, with communication provided through the SIVAM network. This will consist of basic transport services for the following uses:
(a) Transport to the clinic, based upon determined need from representatives from the “mobile clinic”
(b) Transport to more strongly equipped health care facilities for severe cases
3. “Mobile clinic” made up of two to three people (at least one doctor and one health representative) sent to each group on a regular/ non-regular basis (depending upon the desires of the group), to provide the following services:
a) Basic medical care: for injuries and minor illnesses
b) Basic medical education: offered to both the indigenous people as a whole and specifically to traditional healers that can incorporate modern methods into traditional beliefs and methods
c) Hygienic improvements, such as a water filtration system, gradually installed at the request of the tribe (assuming proper funding is attained).
* Note: because all services are optional, each indigenous tribe can choose to receive as many or as few of these services provided *
f) Review Period: (approximately two months)
1. A review board, made up of representatives from both the OPNAH organization itself, and from affiliated groups (such as key donors, and the Brazilian government), will analyze the success of the first three years of the project. Modifications to the plan would be made, based upon problems or successes discovered.
2. Implementation continues.
g) Expansion: (approximately eight years—and beyond for future implementation in other states)
1. Assuming success of the review period, the OPNAH will enter into its second four year Construction/Implementation phase for two more clinics. This will be followed by another review period, and, hopefully, the third and final four-year phase and two month review. While the new projects are implemented, old ones will continue, and mature with changing needs.
2. Assuming success of the project in the state of Amazonas, the project can be expanded into other states, and ultimately become a rainforest-wide organization.
3. With increased credibility, OPNAH will begin to lobby for improved enforcement for health regulations on those entering the region.
h) Program Continues: (indefinite—until stability is reached)
1. A two month analysis of the OPNAH plan will continue every three years
i) Gradual Reduction of Funding will occur as self-sustainability is attained
1. As the indigenous population improves both in numbers and in stability of health, the demands for resources will gradually decrease and funding can be pulled back. With many years of health education provided, tribes will hopefully develop methods of self-sustainable health care and only need basic resources, such as vaccinations and medications. Also, with improved health, indigenous groups will be more able to support themselves in terms of nutrition and other basic necessities. Thus, to some extent, good health can be self-sustainable.
V. Tools and Requirements
a. Manpower:
1. Approximately 24 doctors—four per base station (at first, with subsequent review periods determining actual requirements)
2. At least thirty volunteer workers
b. Funding
1. Possible Sources of Funding Include: Current government finances directed towards indigenous health care (disease control funding was a reported $54 million US in 2001), OPAM, the World Bank, the Pan-American Health Organization, the UN, URIHI, and FUNAI (the National Indian Foundation of Brazil)
2. Projected costs:
(a) $600,000 for clinics ($100,000 per clinic)
(b) In first year (very rough estimates):
$ 200,000 -- for 2 clinics
$ 300,000 -- manpower
$1,500,000 -- supplies (medication, bandages, etc.)
$ 300,000 -- running clinics (energy costs, etc.)
$ 50,000 -- travel (initial analysis, remote region travel, etc.)
--------------
$2,350,000 -- estimated total cost
VI. Testing
To later test the progress and success of the project, a survey group will initially investigate the actual status of the Amazonian region. This will incorporate two main facets. The first is detailed investigation into current information on the status of indigenous groups. Much of this has already been performed through the Mission plan. The second will be physical entry into the region, for purposes of further investigation. This second facet will incorporate interviews, surveys, and gathering of current statistical data. With this information, the OPNAH will then establish a baseline report on the status of indigenous health.
Future testing will then incorporate specific short term and long-term aspects. For short-term analysis, OPNAH will send review panels into each base station region to determine how health has improved, and what specific changes need to be made. These panels will also include members from other affiliated organizations, including, but not limited to, benefactors and indigenous tribe members. Long-term indicators of success include overall marked improved health of indigenous people, and a rising population of indigenous groups.
Specific tests to determine the efficacy will include:
a. Interviewing indigenous people to determine changing health concerns based on increasing and decreasing levels of complaint, and based on:
1. Their views on how the system helps
2. Their specific health concerns (which diseases seem to be more controlled, and which seem to be causing greater affliction)
3. Their views on problems with the system
b. Constant analysis of available government statistics on number of health and disease cases
c. Analysis of changing productivity levels of indigenous groups as the project proceeds
d. Analysis to determine if indigenous groups that initially refused aid begin to ask for it
e. Conducting regular statistical analysis of diseases present, diseases treated, live birth rates, illness-related deaths, and number of cases of serious illness
VII. Expected Results:
If the plan is successful, analysis will reveal a marked decrease in major diseases within the Amazon rainforest region. Based upon the results of past health care efforts (specifically the URIHI plan), a decrease of at least 50% in child mortality and adult death from local diseases would represent adequate improvement in health of the region, and general success of the OPNAH. Complete success would occur with complete eradication of the major local diseases, such as malaria and measles. Also, with complete success of the program, adequate hygiene devices would be provided to every community that wanted it. Finally, if this project is successful, within approximately 15 years, health will have improved to the point that funding to the plan can be safely decreased over time.
VIII. Externalities:
A major obstacle for this plan could be convincing the indigenous people that this aid is indeed useful. From previous analysis and research in the region, it has been determined that many tribes, despite their illnesses, simply wish to be left alone. Because the OPNAH program would be completely optional, it would not encroach upon these wishes. However, this also means that it might be difficult to provide widespread aid to the region.
Another obstacle within the region could be that of internal corruption. While a consistent review board would possibly be able to curb these trends, the possibility for corruption would still exist, and again, might provide an obstacle to program implementation.
Next: International Solution for Sustainable Ranching->
![]()
3: http://www.una-uk.org/brazil2.html
4: Reeve, Mary-Elizabeth. Medical Anthropology Quarterly v. 14 no 1, Mar. 2000, p. 96-108
5: http://www.brazzil.com/p07mar02.htm
6: WorldHealth.org, p.1171
4: http://www.una-uk.org/brazil2.html
5: http://forests.org/articles/reader.asp?linkid=7117
