| Vol.
XXI No.
4 March / April / May 2009 |
| contents |
| Printable Version |
Interview with Director of MIT Medical
Dr. William Kettyle
As with the rest of the Institute, MIT Medical has been hit hard by the economic downturn, being told by the MIT administration that it needs to make budget cuts of 5% per year over the next three years. In a March 26 interview with Medical Director William Kettyle (WK) the Faculty Newsletter (FNL) explored what steps have been taken to meet the first year’s 5% reduction requirement, as well as Dr. Kettyle’s innovative plans for addressing the potential budget reductions in years two and three.
FNL: Thank you for meeting with us. We wanted to try to get a sense of how the budget cut decisions were made at the Medical Center, who made them, and what, if any, faculty input was involved. In addition, perhaps you could address the question of why the Medical Department was cut at all. And, most importantly, what impact the cuts are likely to have on patient care at MIT.
WK: Let me share some thoughts about our approach to the fiscal challenges that we are facing. We can discuss the expense reductions we’ve made for the next fiscal year, and then we can delve into some of the things we are working on and may propose for the following fiscal years.
Our approach is based on our desire to provide the best care and services for this special community. We will do this in the context of the fiscal environment of the Institute.
The Medical Department is many things to many people – in addition to providing care for students and staff and their families; we play a number of other important roles.
What we are at MIT MEDICAL
|
We feel we are a valuable and valued part of the Institute and have an excellent working relationship with the senior administration – something that is extremely valuable given the fiscal stress that we are all facing. We are striving to align services with the needs of our community and with the resources available. In order to find and deploy long-term, resource-conserving, sustainable efficiencies we are, and will be, working closely with colleagues across the Institute.
In the near term, we have been asked to reduce our spending by 5% for the coming fiscal year. We received the same request that the academic departments and administrative areas got – the picture sketched going forward – 5% for 2010 and then an additional 5% for 2011 and another 5% for 2012.
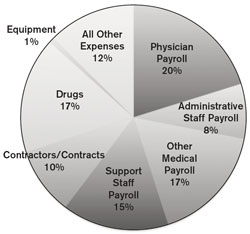
My major concerns are similar to those we discussed five years ago [see “Interview with Medical Director William M. Kettyle,” MIT Faculty Newsletter, Vol. XVI No. 1, September 2003]. We spend 69% of our dollars on people (employees and contractors), about 17% on drugs, and the rest on equipment and support services – what I sometimes refer to as “tongue depressors.” There's a real limit to how much less we can spend on tongue depressors.
We have really put the brakes on pharmaceutical costs. For the last five years we've had an annual increase in expenditures for pharmaceuticals of about 3.7% a year. That's in a world where the rate of increase has been more like 7 to 10% per year. I do not think that we will be able to render any further significant savings in the realm of pharmaceutical expenditures.
MIT Medical Data
|
The potential cost reducing strategies that might apply to the 14% of our expenses that fit into the realm of supplies and purchased services are very unlikely to render significant decreases in our expenses. Of course, we are working to reduce these costs, but we will need to find other sources of savings.
In order to reduce our expense burden to the Institute, we will need to reduce our work force. Unless, and this is a big unless, we can durably increase our revenue. Selling capacity, where we have it, might preserve the scope and scale of services that we provide.
FNL: When you were told about the need to cut the budget was there any pushback?
WK: The “pushback” is the willingness of our department to work with the Institute to find a solution, to find innovative ways to maximize the effectiveness of our resources and to craft an approach that provides and preserves excellent care with thoughtful resource utilization. In the short term, for the next fiscal year, we have found ways to decrease our spending that we feel will have a relatively small impact on the services we provide. There are some things we will do differently. We are sculpting and adjusting our services to maximize the use of our resources.
For example, we were carrying about $500,000 a year in unfilled positions; that number has been roughly the same for the last two or three years. One could make the argument that, since we're getting by without these people now, why do we need to fill those positions.
FNL: That $500,000 was part of your budget?
WK: Yes, but it is no longer.
FNL: How about last year?
WK: We didn't spend it. For a number of reasons several positions went unfilled.
FNL: But could you have spent it on tongue depressors?
WK: No. In general, salary dollars are not fungible across the budget items. There is some flexibility across line items within our budget, but it's not totally fluid.
FNL: Specifically, what type of cutbacks have you had to make for this first 5% reduction?
WK: As I mentioned, the $500,000 allotted for unfilled positions has been removed from our budget. In addition, several clinicians and administrators will be taking two-week, non-paid furloughs. We have also made plans to close the Inpatient Unit for two months during the summer – we call it summer, but it’s really June 15 to August 15. During that time our census has been historically quite low.
FNL: What happens to those patients, or other people who can no longer go there? Where do they go?
WK: It depends on the individual’s situation. Some patients need care to transition them to home following an illness or operation. During the time the Inpatient Unit is closed we will work to try to help them meet their care needs. Others require supportive care that might be available through other arrangements.
FNL: What kind of other arrangements?
WK: Frequent outpatient visits to the department, visiting nurse services, or entering a skilled nursing facility are some of the possibilities.
FNL: Would they have to pay personally for that?
WK: It depends on the specific situation, but some might have to pay for certain services personally.
FNL: But don't people come here to get infusions and things like that?
WK: During the two months that the Inpatient Unit is closed, we will maintain infusion services and other care services. Overnight stays, however, will not be possible. The summer closing of the Inpatient Unit will also mean that there will not be a doctor on site from midnight until 7 am. There will be coverage on site from 7 am to midnight.
FNL: Is this decision reversible at this point in time?
WK: We have begun to make plans to provide the necessary care during the closure of the Inpatient Unit and the reduction in overnight services. We are currently in negotiations with a local hospital and are quite sure that they will be able to provide urgent care services during the night.
FNL: So it's not reversible, but one can go to the hospital instead of coming here.
WK: That's correct. Our patient volume from midnight until 7 am, especially during the summer, is quite low.
FNL: Will you save any money that way? You have to pay the hospital some money for that, right?
WK: Yes, there will be some new, related costs. However, the overall expenses will, we think, be lower – the costs of staffing – two nurses around the clock and a full dietary staff are significant.
| Back to top |
FNL: And what does that do to the nurses and other staff in the Inpatient Unit? I can tell you from personal experience that they are excellent and extremely dedicated. What does it do to their income if they have to take a two-month, non-paid vacation?
WK: Let's talk about that component of the situation. You asked if this is reversible? And that's a very good question and something I've thought a lot about. This is something we considered carefully before we made any changes.
Most of the personnel changes, although not all, for the coming year are in the form of furloughs – vacations without pay. The jobs in question remain in our system, but we will experience a temporary decrease in salary expenses. So the changes are “reversible” in that they are not destructive.
Furloughing – if I can use that word as a verb – is a temporary way of decreasing expenses while we find more durable, long-term solutions. They buy time. The word “vacation” is clearly not appropriate. A furlough is not working and not getting paid. All employees on furlough will continue to receive benefits, however. Benefits are not shut off.
But for the nurses and the dietary workers in our Inpatient Unit it means two months off in the summer without pay. For some, that means “Gosh, I can play golf every day” or “I can spend the summer with my kids.” But for others it means “Oh my gosh, we were having trouble covering the mortgage payments before this happened. How am I going to keep my house?” That's the most painful situation. Unfortunately, some may feel forced to seek employment elsewhere. We run the risk of losing nurses and dietary staff who are highly skilled and devoted to our patients and our community.
I've spent some time with the nurses and dietary staff, and I don't know how it will come out in the end. I think it will work out OK for most of them and I hope we won’t be losing people. Still, I realize that it has to be difficult to have an unplanned, unpaid “vacation.”
FNL: MIT's a pretty good place to work.
WK: It is an excellent place to work, and we’re hoping that will compensate in some way for the loss of income.
FNL: In other areas how did you decide who will and who won't have to take a furlough?
WK: The decisions were made on a service by service basis, taking patient needs, seasonal variations in demand, availability of coverage and other factors into consideration. There will, for example, be no furloughs in our OB/GYN service. Their demand is high and decreasing staff time would lead to unacceptable cuts in appointment availability.
FNL: Dermatology I would think would be similar.
WK: Dermatology is similar. And there are no furloughs in Pediatrics. Each of the internists will take a two-week furlough. The furloughs are being scheduled carefully so that the number of clinicians that are on site at any given time will meet the demands for care.
FNL: And what about salary cuts? How were those decided?
WK: There are no salary cuts other than the furloughs. For most of the furloughs, however, it is a functional salary cut.
FNL: And what about salary increases?
WK: We’re freezing salaries for everyone with the exception of people who make $75,000 or less.
FNL: That’s similar to what it is in the academic and administrative units. That's for year one?
WK: That's for year one.
| Back to top |
FNL: How do you plan to approach the challenges for FY2011 and 2012?
WK: We are approaching the subsequent fiscal years with energy, with ideas and with a spirit of cooperation – cooperation with the leadership of the Institute and with our colleagues across the Institute. Why don't I outline what we are doing?
As you know, a task force – the MIT Institute-wide Planning Task Force – has been established to generate ideas and problem-solving strategies. There are nearly 200 people involved in nine or 10 subgroups. It’s a big group. One of those subgroups is focused on Human Resources and Benefits – medical care issues fit clearly into that group. We also see ourselves as important players in the provision of a healthy and safe environment for our students and will be meeting with the subgroup on Student Life.
My major concerns for fiscal years 2011 and 2012 have to do with the potential transfer of care and costs out of the Medical Department. If we do less here at the Medical Department because of budget limitations, we will be care-shifting and cost-shifting to the outside world – to the medical community around us – where the costs may be lower, the same or, in many cases, I think, higher. The overall cost savings in health care expenditures for the Institute and its employees and students might be very small or, indeed, non-existent.
Each potential shift of care will need to be analyzed carefully to assess the effect on overall health care spending. The quality and integration of shifted care might be fine, but in many areas I suspect it will not be as good or as well coordinated. Contracting the Medical Department may not save the Institute very much money.
FNL: Didn’t you make a presentation to the subgroup on Human Resources and Benefits a little while ago?
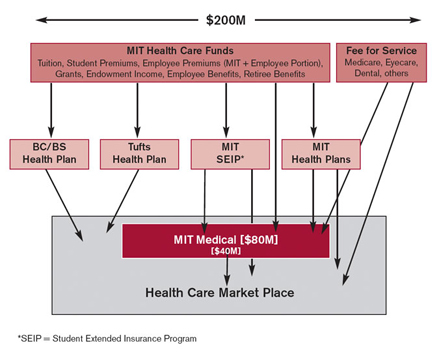
WK: Yes, I did, about 10 days ago. Basically, what I said was that there is nearly $200 million spent on health care globally by the Institute community. This large sum is the total spent and includes funds that MIT contributes to employee health insurance; it includes the funds that we, as employees, pay for our portion of the health insurance premium; it includes the co-pays; it includes the portion of tuition that is earmarked for student health care; it includes money spent for retiree health care.
About $80 million of that $200 million comes to the Medical Department – about $40 million stays here and pays for the salaries, for the contractors, for the drugs and for the tongue depressors. The additional $40 million that comes to us really goes through us to pay bills at any one of a number of places where we buy services for our patients.
FNL: What about reimbursements made by Blue Cross/Blue Shield?
WK: Blue Cross/Blue Shield of Massachusetts plays two important roles in the administration of health care funds at MIT. The insurance programs, managed by the MIT Medical Department, use Blue Cross as an ASO – Administrative Services Only – agent to pay our bills for services obtained by our patients outside the Medical Department. This allows us to take advantage of the preferred rates that Blue Cross has negotiated with providers.
Through separate arrangements with Blue Cross and with Tufts Health Plan, the Institute purchases health care services for employees and their families who are not members of the MIT Medical Department plans. In these cases Blue Cross and Tufts Health Plan also function as ASO agents – again taking advantage of the contracts that these companies have with providers, thereby limiting the costs of care.
FNL: But does Blue Cross/Blue Shield or some other organization out there actually put any money into the health care of the MIT community?
WK: No, MIT is self-insured for health care programs. The Medical Department provides care on site and Blue Cross and Blue Shield and Tufts Health Plan provide administrative services that allow MIT to purchase services at discounted rates from medical care suppliers outside the Medical Department.
FNL: So if a physician or someone providing care in the community charges say $100 for some procedure and the patient gets a note saying that $50 has been allowed by Blue Cross/Blue Shield and the balance to the patient is zero, is it that the other $50 is collected by the physician, or does somebody else pay?
WK: In some cases there may be a deductible or co-payment that is the responsibility of the patient. Most of the time, however, because “balance billing” is not allowed in Massachusetts, the provider must settle for the “allowed” amount. So the bill for a $100 service is deemed to be worth $50. This is an example of the utility (for the payer, not the clinician!) and power of the contracted network that has been established by Blue Cross. These contracts together with the lack of “balance billing” mean that transactions are settled at amounts that are significantly lower than the “sticker price.”
The Institute rents – actually, that's the term used in the business – rents those contracts to pay $50 instead of $100 for that service. So we get a significantly discounted rate. At MIT Medical we also use Blue Cross as a payment vehicle in order to take advantage of their contracts with area providers. The $40 million that goes through us goes through us typically via Blue Cross arrangements. We pay Blue Cross an administrative fee; they, in turn, pay our bills and we reimburse them for those payments.
The other $120 million spent on health care doesn't come to us or go through us. Some of those funds could be a source of income for the Medical Department. We do have some capacity in some areas – capacity that might allow some of the revenue that is leaving the Institute to remain on campus.
One example is mammography. About two years ago we bought a state-of-the-art mammography machine. The machine is capable of handling ~4,000 mammograms a year. We currently do about 2,000 studies a year. If we opened up the availability of convenient, on-campus mammography for members of our community who are not members of our health plans, some of the flow of health care funds currently being spent outside of MIT could remain on campus to support our activities.
FNL: I wonder about the size of the Task Force. On the face of it, a 200-person Task Force sounds excessive. But if it can deal with all the different levels of pay that are being cut throughout the Institute in some effective way, then maybe it's a good thing.
WK: Although the Task Force is large, it is well designed, well staffed, and well managed. The range of areas, options, and issues to be considered is huge and I think a large group is necessary. The subgroups are co-chaired typically by a faculty member and an administrative leader. There's been some significant craft put into designing the Task Force and into the selection of the people – these 200 people. I think it will work well.
FNL: And years two and year three are disasters?
WK: I hope not! It will be difficult, but with the help of the Task Force and our dedicated staff I think we will find ways to provide the care and support required to meet the mission of MIT.
Furloughs are clearly a temporary way of reducing salary expenses. They buy us some time while we search for solutions. We have not dismantled services and I hope we will not have to going forward. I think we must durably increase our revenue stream while at the same time work to trim expenses. Sculpting and shaping the services we provide to the needs of our community with the resources available are our current foci. Unless we are able to significantly and durably expand our revenue stream, we will be forced to make significant cuts in personnel.
The other important thing that's happened over the past few years is the full deployment and development of self-insurance for medical care at the Institute. Self-insurance increases flexibility in the system, and opens options.
FNL: How do you anticipate MIT Medical responding to President Obama’s plans for national health care?
WK: I'm a strong proponent of improving the structure of health care. And I think we, as an educational institution, will be able to find a comfortable position in an improved system of health care delivery.
FNL: As a provider?
WK: Yes. I think that the Medical Department will fit very nicely into some of the proposed approaches. So I'm enthusiastic. I think the Obama Administration's interest in the electronic aspects of providing and managing care is something we have a head start on. Our electronic medical record system and our Patient-On-Line portal are two good examples. In addition, we have highly effective analytic tools that help enhance quality and allow us to monitor expenses.
We have developed “dashboards” which are a very nice demonstration of how technology can improve care. For example, we can now easily determine the frequency of appropriate pneumococcal vaccination in our practice. This can be broken down by provider and, most importantly, the systems allow the provider to “drill” into his or her data and identify those patients needing immunization. Arrangements can then be made to bring the immunization status up to date. This technology is on my desktop computer and is very easy to use. This is a clear example of technology enhancing care. Similarly, it can be used with other items of care, such as mammograms and colonoscopies; so I am a great believer in the use of information technology – to enhance patient care.
FNL: Information Technology funds haven't been cut in the first 5%?
WK: No, we have not cut funding for IT.
FNL: Anything else you’d like to say?
WK: The situation is very different than it was five years ago.
FNL: Better?
WK: Better. Much better. It feels very different because I think we have a coordinated, cross-Institute planning and evaluation process in place. In addition, at the Medical Department we have a much better, a much broader, and a much deeper understanding of the business basis of our operations. From a fiscal point of view, we understand things much better -- something which I think is critical. We’ve learned a lot.
Most importantly, I think that the senior administration has a keen appreciation of the role and the value of the Medical Department. The approach of looking broadly at the provision of health care and wellness services across the Institute will lead to better care, better health, and better use of our resources.
Thanks for giving me this opportunity to share our progress and our plans.
FNL: Thank you.
| Back to top | |
| Send your comments |
| home this issue archives editorial board contact us faculty website |