
| Vol.
XVIII No.
2 November / December 2005 |
| contents |
| Printable Version |
Medical Task Force Releases Final Report
After more than a year of work, the Task Force on Medical Care for the MIT Community released its final report in early November. The Task Force examined all aspects of medical care, medical insurance, and related educational and community support programs available to MIT students, employees, retirees, and post-docs through the MIT Medical Department, as well as through outside health insurance programs administered by Blue Cross/Blue Shield, Tufts Health Plan, and Delta Dental.
The Task Force concluded that the existing MIT model for providing health care and health insurance has performed well historically, that the MIT community is generally highly satisfied with it (see M.I.T. Numbers), and that it can continue to serve MIT well in the future if various reforms are implemented. The final report offers over 40 recommendations aimed at improving access to and quality of health care provided by the MIT Medical Department, improving satisfaction with health insurance options, reducing the cost of providing health care and health insurance, and enhancing "wellness" and related health care education initiatives. "We believe that some of these recommendations require urgent attention by the MIT Administration. Others are less urgent but should be part of a comprehensive longer term implementation strategy to ensure that our health care and health insurance policies are compatible with the pursuit of MIT's primary goals for excellence in education, research, and service to society."
Created by former president Charles Vest in September 2004, the members of the Task Force included faculty, staff, and students. It was chaired by Professor Paul L. Joskow, Elizabeth and James Killian Professor of Economics and Management. The Task Force was charged to examine all aspects of the costs and quality of medical services and health insurance coverage provided by MIT to its students, employees, retirees, and post-docs, to solicit the views of all segments of the MIT community, to examine alternative models for providing health care, to develop a vision for the future of medical care and medical insurance at MIT, and to make recommendations to realize this vision.
In response to this ambitious charge, the Task Force conducted analyses of the costs of providing medical care and medical insurance through the MIT Medical Department, the costs of care provided through outside insurance options, developed various comparative benchmarks of the quality of MIT's health insurance benefits programs and their costs, conducted surveys of students, employees, and faculty retirees regarding their satisfaction with the health care and health insurance available to them. Members of the Task Force interviewed physicians and nurses employed by the Medical Department (present and past). The task force received input from the MIT Medical Management Board and the Medical Consumers' Advisory Council and received numerous confidential communications from employees, members of their families, and current and former staff of the MIT Medical Department.
| Back to top |
Task Force Recommendations
An important component of the Task Force's work was the consideration of alternative models for providing health care and health insurance to the MIT community. After careful consideration of the costs and benefits of alternatives and the views of the MIT community, the Task Force came to a unanimous conclusion: "The Task Force recommends that MIT continue to support our longstanding existing basic model for medical insurance and medical care delivery. It has served the community well. It has been damaged somewhat by arbitrary and excessive budget cuts and imperfections in the way they were managed. The focus should be on improving the quality and cost effectiveness of this model and MIT's ability to put in place more effective financial management and governance arrangements."
In arriving at this conclusion, the Task Force compared the costs of providing medical care by the MIT Medical Department through the MIT Health Plans to the costs of the Blue Cross/Blue Shield and Tufts Health Plans. Roughly 55% of MIT employees on the Cambridge campus belong to the MIT Health Plan, including nearly 80% of the faculty. The other 45% of MIT employees are enrolled in one of the Blue Cross/Blue Shield plans or the Tufts Health Plan . "The analyses performed at the request of the Task Force suggest that on a risk-adjusted basis, the care provided by the MIT Medical Department is no more expensive, and may be less expensive, than care provided under the BC/BS and Tufts plans." Thus, the perception that providing employee care through the MIT Medical Department is more costly than the alternatives is not consistent with the facts.
The 40 recommendations made by the Task Force to improve the quality and cost effectiveness of the "MIT Model" include:
1. The MIT administration should express its confidence in and strong support of the MIT Medical Department and its goals. Events over the last few years have created uncertainty about MIT's confidence in the Medical Department and the future of the MIT Health Plans for employees. These uncertainties should be resolved by a definitive support for the central role of the MIT Medical Department in providing health care to the MIT community.
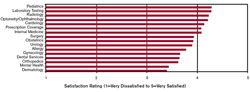 Faculty Satisfaction with Individual Service Areas (click on image to enlarge)
Faculty Satisfaction with Individual Service Areas (click on image to enlarge)2. There is an urgent need to add resources to the Medical Department's budget quickly to improve access to care and to provide the time and resources required by caregivers to deliver high quality care. The Task Force did not want to micromanage the delivery of care by the Medical Department but identified several areas where consideration should be given to adding or redeploying some resources. These areas include: internal medicine, dermatology, OB/Gyn, pediatrics, urgent care, clinical staff support, and mental health care provided to employees. The Task Force recommends that the Medical Department submit a plan to the administration within 60 days, along with a budget and evaluation of how any additional costs will be recovered.
The recommendation to add resources to the Medical Department should not be interpreted as a strategy of "back to the past." The U.S. health care system is dynamic and is characterized by rapidly increasing costs. MIT must continue to adapt to these changes and to find ways to improve the cost effectiveness of care provided by the Medical Department as well as care provided through outside insurance plans.
3. Improve central MIT administration's budgeting and financial management framework for the Medical Department. The Task Force concluded that the budgeting and financial management protocols applied by MIT to the Medical Department have serious deficiencies. The report outlines a new budgeting template for the Medical Department that it recommends the MIT administration use for budgeting and financing management purposes. Complementary efforts to improve and integrate the MIT Medical Department's internal budgeting and financial managements systems and improved governance arrangements for the Medical Department are also recommended.
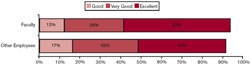 Overall Rating of Primary Care Physician (click on image to enlarge)
Overall Rating of Primary Care Physician (click on image to enlarge)4. Continue efforts to identify and take advantage of opportunities for reducing costs or increasing productivity without reducing the quality of care in the Medical Department. Specific areas discussed in the report include the infirmary, medical laboratory, dental service, pharmacy, and the use of modern information technology. Increased investment in and use of modern information and communication technology in particular can improve the quality, expand access to care and reduce the costs of medical records, facilitate exchanges of medical information within the department and with outside providers, and help assessments of objective measures of the quality of care.
5. Expand the participation of the Medical Department in MIT's educational, wellness, environmental, health and safety initiatives, and community outreach programs. MIT's wellness programs are not up to best practice in industry. Good wellness and related educational programs can improve the quality of life of students, employees and retirees and reduce health care costs in the long run.
6. Evaluate whether and how MIT can make more effective use of the resources available in the Boston medical community by developing a closer partnership with one of Boston's major hospital groups .
7. Improve education about the availability and effective utilization of mental health care services for students and respond to some students' negative perceptions and concerns about the mental health service. More generally, improve education about student medical benefits, the "smart use" of the MIT Medical Department and the external Boston area health care system for our students.
8. Strengthen MIT's capabilities to implement its self-insurance strategy for setting insurance premiums and controlling the costs of care provided through the Blue Cross/Blue Shield plans, the Tufts Health Plan, and Medicare supplement plans. MIT spends (before employee contributions) over $50 million per year on services provided through these plans. The costs of these plans require comparable attention to the costs of the Medical Department. More effective management can reduce costs.
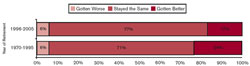 Quality of Care Since Retirement
Quality of Care Since Retirement
(click on image to enlarge)9. Phase in changes in the way health insurance premiums are set consistent with the recommendations of the Strategic Review of Benefits Committee. The proposal to reflect improved risk pooling and adjustments for demographic differences across health insurance plans can be implemented as soon as possible. The proposals to create alternatives to traditional family coverage and wage-related premiums were more controversial and would benefit from additional analysis and consultation with the MIT community.
10. Consider offering a high deductible and high co-payment insurance option and a Health Savings Accounts program for employees.
Conclusion
The entire final report of the Task Force on Medical Care for the MIT Community can be found at: web.mit.edu/task-force/medical. As is abundantly clear from both the surveys and many interviews, the availability of high quality and convenient medical care at a reasonable cost is important to all segments of the MIT community. Consistent with the conclusions of the Committee on Faculty Quality of Life (MIT Faculty Newsletter, March/April 2005, page 7), it is also clear that the vast majority of the MIT faculty place a high value on the availability of health care at the MIT Medical Department and that reducing the availability and quality of these services would be considered to be a major reduction in the quality of life of Institute faculty members.
Preparation of this article included contributions by Prof. Paul Joskow, Mandy Smith, and Janet Snover. Charts used were prepared by members of the Office of the Provost/Institutional Research, from surveys commissioned by the Task Force on Medical Care for the MIT Community. These online surveys were administered by Jag Patel and Jeff Schiller of IS&T.
| Back to top | |
| Send your comments |
| home this issue archives editorial board contact us faculty website |